I am already overwhelmed and humbled by the response to my last blog post. The multitude of friends who have had bumps along the road in their own breastfeeding journeys reaffirms why we need to be talking about this. I promised a follow-up with the specific details of my breastfeeding journey. It’s longer than I anticipated, but I wanted to remember the details while I still could. And I had a friend message me today with questions about a situation similar to mine, so I wrote this in a hurry for her. So here goes…
My daughter’s first breastfeed during our golden hour after birth was more like a breast-lick. She never really got latched on in the delivery room, but I didn’t have time to worry about it. I was in the middle of a postpartum hemorrhage, and she had to be taken off my chest so that they could more effectively massage my belly down. Truthfully, it was all a haze.
After we were transferred to our postpartum room, our attempt at breastfeeding started in earnest. Immediately she was screaming while I tried to get her latched. My nurse stacked some pillows up, sandwiched my boob in her hand, and tried to shove it into my daughter’s tiny mouth. She stayed on for maybe a minute, then popped off. Try again. On. Off. Try again. On. Off. So went the next 4 hours of cluster feeding. In between each “feed” my fingers were flying across my phone’s keyboard, desperately trying to figure out what might be going on. I knew she wasn’t getting much, if anything. She wasn’t content at all, she was just falling asleep in between feeds from exhaustion. Nothing about her latch was correct. She couldn’t open her mouth wide enough to get deep enough, and her upper lip was never able to flange out. At 3 am, about 12 hours after her birth, I buzzed the nurse practically in tears. I need a spoon. Show me how to hand express.
I expressed my liquid gold into a plastic spoon and my daughter gulped it down. Ahhhh. I could finally feel us both relax a little bit. First thing in the morning, she was taken away briefly for her pediatrician exam. A little while later the pediatrician came to my room and discussed his exam. Everything’s great, she’s perfectly healthy. But she’s lost 7% of her birth weight already, so we need to keep an eye on that. 7%? Already?? I thought we’d have more time to figure this out.
Shortly afterwards, a lactation consultant came to see us. Oh thank God you’re here, help us. She reviewed our chart and the pediatrician’s notes. Your pediatrician has suggested formula supplementation due to weight loss. What? Already? You’ve got to be kidding me. It’s been less than 24 hours, and you’re already giving up on me?
She observed our feeding, and wrinkled her nose a bit. I’m going to come back again in a few hours to watch you again. She rolled in a hospital-grade pump and showed me how to use it. I hadn’t brought my hands-free bra to the hospital, so I had to hold the flanges up while I pumped. I didn’t care though – at that moment, I was supremely grateful for technology. This amazing thing called the breast pump would save me. More liquid gold. More gulping. More relief.
A few hours later the lactation consultant came back and observed us again. Afterwards she stuck her finger in my baby’s mouth and felt around. She has a bubble palate. Your nipple isn’t long enough to hit her palate and stimulate her sucking reflex. So you’re basically telling me that my body is incompatible with my baby’s? How is that even possible? I didn’t even know that was a thing. She provided no explanation, she just said it matter-of-factly and then pulled out a nipple shield – think of it like a little silicone sombrero for your nipple. The idea was that it would help “reach” her high palate and trigger her sucking reflex better. We tried the shield for the next few feedings – and while it made it less painful on me, it didn’t seem to make my baby’s latch any better. She continued her pop on, pop off routine. I asked the LC about why my baby’s lip wouldn’t flange out, because I knew that was a key to making a tight seal. She just shrugged her shoulders and told me I needed to keep flipping it out manually until she learned that was the way it was supposed to be. Despite all of my manual manipulations, her lip always returned right back to where it was.
We survived another night, struggling with latching, pumping, and spoon-feeding, with a revolving door of postpartum nurses who would pull and prod at my breasts. The next day before discharge, I desperately asked the LC – If she’s still not latching well once my milk comes in, what should I do?
This is the moment where this first lactation consultant failed me. She could have observed that the pump flanges she had given me were not the right size, and that they’d eventually contribute to sore and cracked nipples. She could have suggested syringe feeding so that we could avoid nipple confusion. She could have told me about paced bottle feeding so that my baby wouldn’t develop a flow preference. She could have introduced me to the idea of a Supplemental Nursing System (SNS) to help keep my baby happy & full at the breast, and prevent a breast aversion. She could have told me that there was probably more to the story than just the bubble palate. She could have suggested I go ahead and make an outpatient appointment for lactation, that they’d be able to tell me more after we did some before & after feeding weighs to see how she was transferring milk. She could have told me that the earliest appointments available for lactation were at least 14 days out. 14 days is a lifetime in a nursing relationship – that’s at least 112 feeds.
Instead, in this moment when she could have said so much, she handed me a bag filled with disposable bottle nipples. It spoke louder than all of the things she could have said. A screaming vote of no-confidence. A lactation consultant, a trained professional who was supposed know about breastfeeding, was essentially telling me that she didn’t think there was another way besides the bottle.
And then literally moments later, the nurse walked in with my discharge paperwork and a “gift bag” to send me home with. Inside this bag were some pamphlets, and a 4-pack of formula bottles. I was hearing the message loud and clear: We don’t know how else to help you, and now you’re on your own. No wonder so many women quit breastfeeding before they even leave the hospital.
Once we were home, we tried just nursing the entire first night. By morning, my nipples looked like a new tube of lipstick, but raw and cracked, and my baby was not content. However, my milk had come in, so spoon feeding didn’t seem like it was an efficient option anymore. I reluctantly reached for that first disposable bottle nipple and screwed it onto the first bottle of milk I had pumped. I hadn’t planned on introducing a bottle for at least 3 weeks; everything I had read said that I needed to establish breastfeeding first. But when your baby is eating every 2 hours, for an hour at a time, there’s no time to figure out another solution on the fly. The first priority is always to feed the baby.
Our pediatrician’s visit on day 3 indicated that she had lost 10% of her birth weight. However, I assured the pediatrician that we’d get it turned around; my milk had come in, and now we could ensure she was getting it. She said I wouldn’t have to supplement if I’d come in for weight checks every other day until she was back up to birth weight. There was that threat of formula supplementation again, without any suggestions of what else to do. I was resolved to do whatever it took to avoid it – my body was making milk.
So we settled into a new normal; I ordered more pumping parts (this time sized correctly) on Amazon (thank God for Prime), and started pumping around the clock. Baby would nurse, then I would pump, then I would feed the pumped milk in a bottle. Maybe a 30 minute or hour break, and then repeat. Breaks were mostly devoted to self-care; recovering from a bad tear & postpartum hemorrhage are no joke. I had lost so much blood that I needed to take iron supplements to keep my energy up.
Soon I got 1 bottle ahead, and the routine changed a bit. Baby would nurse, I’d feed the bottle I pumped the previous session, and then pump for the next feed. Eventually I got coordinated enough to feed a bottle and pump at the same time. Eight times a day on days I felt I was making enough milk, 10 times per day on days I got nervous about my milk supply, 12 times per day during growth spurts. I mimicked her feeding pattern – if she ate, I pumped. My sweet husband washed all of the bottles and pump parts several times a day, changed diapers, ensured I remained fed and hydrated, and comforted me whenever I fell apart. Soon my daughter was back at birth weight and climbing.
I read everything I could on milk supply and pumping (thank God for kellymom.com). If I couldn’t successfully nurse my baby, then I was determined to kick ass at this making milk thing. I did everything I could to reduce my stress and relax (by binge watching Arrested Development in 15 minute increments). I learned how prolactin levels are highest between 1 and 5 am, and how activating prolactin receptors is the key to long-term milk supply. So I set my alarm for 1, 3, and 5 am, and diligently pumped. I learned about power pumping, and did 10-minute on / 10-minute off sessions for an hour during baby’s naps. I took fenugreek supplements and my supply practically doubled overnight. I learned about how to massage while pumping, and doubled it again.
It was the hardest thing I had ever done in my life. And that’s saying something, considering the fact that I had just given birth to a 10 pound baby without drugs. This was much harder. All jokes aside though, my birth actually had a large role to play here. Whenever I felt like I couldn’t do it anymore, when I wanted to just sleep through my next date with my pump, I drew strength from my birth. If I could do that, I can do anything. My birth had unleashed a power inside of me that I didn’t know existed. It made me ferocious and confident in my motherhood. Besides, this was my job right now. To feed my daughter. This was a brief moment in time, and I was going to figure it out.
I should note that bottle-feeding was not going great. My daughter still couldn’t flange her lip out, which meant she couldn’t get a tight seal on the bottle, which meant she was getting lots of air, and lots of milk was dribbling out of her mouth. And her high palate meant that I had to constantly keep an eye on the bottle to make sure she hadn’t compressed it to the point where nothing could come out. We tried at least 5 bottle types before finding one that she couldn’t compress. Unfortunately, my nipples were not so lucky.
2 weeks in, I finally had an outpatient lactation appointment, this time with a different consultant. We weighed my baby before I nursed, she nursed for 30 minutes, and then we weighed her again.
½ an ounce. In 30 minutes. My heart sank. I was making plenty of milk; she just couldn’t transfer it efficiently.
The lactation consultant suggested that I rent a scale for a week and see if it was just a fluke, or if it was a consistent issue. She also confirmed that the issue was likely due to a high palate, and suggested that I wear soft shells in between feedings to help draw out my nipples more.
I weighed her before and after nursing sessions for the next week. The story was the same every time. 30 minutes. 0.4 ounces. 0.5 ounces. Never more than 0.6 ounces. I went back to lactation, returned the scale, and hoped for another suggestion. The LC thought that my baby could benefit from occupational therapy to strengthen her suck. Another week went by before I could get in to see the OT. She gave me some tongue exercises to do with my daughter, and told me to start doing suck training with a gumdrop pacifier. None of this added up to me. But why does she have a weak suck? She wasn’t born prematurely, she was 10 pounds for crying out loud.
Suck training made the problem even clearer to me. My daughter couldn’t hold a pacifier in her mouth for longer than 10 seconds on her own. It kept popping out of her mouth, much like my breast would. The tongue exercises would quickly exhaust her, and it was obvious that she had very little mobility with her tongue. And besides being exhausted, she was angry. She was starting to scream at my breast, and physically push me away. She hated nursing, and I started to dread it. I remember collapsing into my husband’s arms one day, sobbing she hates me. I stopped trying to nurse at night, it was too much for both us – I just pumped and bottle fed. During the day I’d bring her to the breast after her bottle, and tried to associate the feeling of being full and happy with the feeling of being snuggled up to me. We were skin-to-skin constantly. And when she wasn’t in the nursing position, she was the happiest baby you’ve ever met.
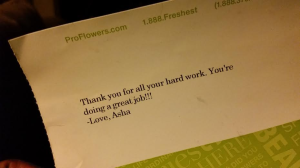
One thing kept me going at this point: surprise flowers with a note from my daughter. It took me a week to figure out which friend had sent them to me. This note held so much power for me, and I’m eternally grateful for this friendship.
Another OT appointment came and went. The LC at that appointment (a new one to me), was surprised that I had still managed to avoid formula. You know, pumping may not be sustainable long term. My pediatrician basically said the same thing to me that same week. Lady, I’ve made it this far, and I’m tired of people telling me what I’m capable of doing.
My abundant supply did not come without its costs. I frequently suffered from painful clogged ducts that would trap me inside the house all day while I tried to relieve them. Once again, I learned all I could about how to work them out, and eventually got them under control with a few key tips (lecithin supplements, rice socks as compresses, pumping after hot showers, pumping at different angles, no bra around the house.)
Week 5: I finally got unchained from my pump for long enough to make it to the breastfeeding support group that they had told me about at lactation. It was my lucky day; it was the last group that was being led by a veteran LC who was retiring. There were also several other LCs in the room, but they were there as mothers to their own little ones. I was so nervous to speak and share my story because I was afraid that I would start crying before I could spit it all out. When I finally re-lived what the last 5 weeks had held, their words surrounded me like a warm hug. What you’re doing is amazing. You should be proud of yourself. We know you can do it. I didn’t know it, but it’s what I had been waiting for. For someone with authority to tell me I was doing the right thing. Doing a good job. To have confidence in me. None of my pediatricians, lactation consultants, or occupational therapists had said anything like that to me. All of their doubt was erased in a single day by the words from this room of amazing women. Why couldn’t one of you have been my lactation consultant?
And then the answer came. She might be tongue-tied. They’re sometimes hard to diagnose if it’s not an anterior tie. She might have a posterior tie. It’s the kind of thing you can have evaluated by a Pediatric ENT, and they can clip the tie, releasing the restriction on her tongue, and allowing it to become more mobile. They’re often accompanied by upper lip ties and high palates. And if she’s still willing to latch, you also might want to consider using an SNS to try to avoid breast aversion.
Yes. Yes. Yes. That night I read all about tongue-tie. I compared the symptoms with what I was experiencing. Check. I compared the pictures with what my daughter’s tongue and upper lip looked like. Check. I called and made an appointment with a Pediatric ENT. We’d have to wait 2 weeks. Damn.
While we waited for our ENT appointment, we went to lactation again. My daughter was still willing to latch, but it was clear that she was developing a bottle preference and a breast aversion. I asked about trying an SNS, but was met with skepticism. They’re really finicky to use. We typically only recommend them for people who need to build more supply, and you have plenty of milk. And she’ll be taking bottles when you go back to work anyways, so let her get more practice with the bottle. I left feeling defeated again, but hopeful for answers at the ENT.
But by the time our appointment rolled around in week 7, it was too late. My daughter had developed a full-fledged breast aversion. She screamed every time and pushed me away. I’m glad that we went ahead with the revision of her posterior tongue tie and upper lip tie. The procedure (in-office, local anesthetic, quick snip to the tight frenulum under her upper lip and her tongue) allowed her to bottle feed more easily. She could finally flange out her upper lip and keep a tight seal. She could finally keep her pacifier in. She could drink from the bottle faster than she ever had before. I knew in the future it would help prevent dental and speech problems. Her tongue had been freed. And I had the answer I had been looking for all along.
I’ll never know for sure if it could have saved our nursing relationship had it been diagnosed earlier. But in my heart I know it would have. A few days after the procedure, I marched into my final lactation appointment and demanded to use an SNS. But my daughter wouldn’t latch on for long enough to give it a chance. I walked out of there angry and resentful. They should have seen it. They should have supported keeping her at the breast. They should have known their own limitations and referred me earlier.
At 10 weeks I finally decided to stop torturing both of us, and stopped trying to nurse. I decided to become an exclusive pumper, for the sake of my relationship with my daughter. I’ll never forget the last time she nursed. I tricked her – she was still asleep, and so I attempted nursing in a side-lying position on the bed with her. I started with the shield so that she’d think it was a bottle, and then slipped the shield off. She was sleepy enough to nurse peacefully for 10 minutes. I’ll remember those 10 minutes forever. But then she woke up and pushed me away. It was the last time I’d put her in a situation to push me away.
I eventually came to peace with my decision. Not trying to nurse her anymore saved me hours each day, not to mention heartache. Our bond grew quickly, in large part due to bedsharing (which is another journey for another post), and I actually got to enjoy the rest of my maternity leave. At 12 weeks I finally felt confident enough in my supply to drop from 8 pumps a day to 7. By the time I went back to work at 17 weeks, I was down to 4 pumps a day, without losing any output. When she started on solid food at 6 months, I was down to 3 pumps per day, and still making enough to put 2 bottles per day in the freezer. It almost felt unfair – somehow exclusively pumping had made it easier on me than on my friends who were nursing. They had to nurse morning and night, and then pump 3 times during their work day, and were struggling to keep up. I donated milk to two such mothers. This time around I plan on donating any extra milk I make to a milk bank that serves NICUs. But even though pumping became easier, I desperately wished I could have nursed.
Stopping pumping was more emotional than I thought it would be. 12 months rolled around and I wasn’t ready. I even switched daycares because our original one wouldn’t allow breastmilk in the toddler room. Like hell you’re going to tell me when I have to wean. I fought for this. My daughter could sign for milk, and asked for it while she watched me pump. She knew where her milk came from, and that meant the world to me. But I still hadn’t gotten my cycle back, and I wanted to get pregnant again. I pumped for the last time on the day she turned 16 months old. It’s been over a year since I pumped, but since I became pregnant, she has asked me for my milk 3 times. It’s amazing that she remembers, and even more amazing that she can sense / smell that my milk is back now, preparing for her baby brother.
I know that I’m one of the lucky ones. I was lucky that I didn’t suffer from postpartum depression. I was lucky to have a husband that supported me. I was lucky to be able to afford a good pump, extra pumping supplies, lactation support, and enough unpaid time off of work to be able to figure it out. I was lucky to have a workplace that supported pumping. I was lucky to have a work schedule that accommodated pumping. But it’s sad to me that we have to fight so hard for something that should be supported more in our society.
I feel hopeful for my next breastfeeding journey. I have confidence. I have a plan. I have a new pediatrician who understands breastfeeding. I now know more great lactation consultants than I can count. I’m armed with more breastfeeding knowledge than I know what to do with. But I also know that I could encounter an entirely new set of issues. Maybe my son will be the type of baby who refuses bottles. Maybe I’ll get mastitis. Maybe he’ll have reflux. Maybe he’ll have a dairy allergy. Who knows? But now I have a village. A village filled with a lot of seriously kick-ass mothers who will help me fight whatever I’m up against.
We all have our own journeys. What worked for me may not work for you. But if you’re a new mother reading this: This is a time-sensitive issue. Find help quickly. I hope you find your village in time.
*In addition to an in-person support group, I highly recommend finding a closed Facebook group you can join. There are a ton out there, and there’s nothing more helpful than other moms who are also up at 3 am nursing their babes to help you with your questions. The larger the village, the more likely you’ll be to find someone who has experienced your specific issue.

Thank you for putting this into words. I cried while I read it because I had such a similar experience. I feel like exclusively pumping has been the most challenging thing I have ever done. It is not understood by the medical community and I have been put down by my own health care providers because I really need to “try harder” or reintroduce the breast. No one will ever understand what this journey is like unless you have been there yourself. Good job mama!
LikeLike
oh my… I was not prepared for tears when I started reading this! I have seen a lot of women voice their frustration at not being able to nurse but never have I seen the hurt, determination, frustration, defeat, and love put together so beautifully. I had to chuckle at if your son will refuse bottles – wouldn’t that be ironic?! Best of luck to you!
LikeLike
This brought back a flood of memories for me! My first was a preemie and had difficulty latching and figuring out the suck, swallow breathe. I also had postpartum hemorrhaging. I didn’t have very good support and ended up bottle feeding quickly to try to get him to gain and then he developed the breast aversion and bottle preference. I remember the tears all to well and finally giving up at trying to put him to breast. Good for you momma for exclusively pumping so long! I made it to between 5 and 6 months and then my son ended up in the hospital and my supply tanked and I didn’t know what to do at the time. However I did want to offer the support that my second son is now 14.5 weeks old and breastfeeds a like a champ and makes it very clear he would rather have the breast than the bottle! The online group and a different lactation consultant have made a world of difference! Best wishes with baby number 2!
LikeLike
Pingback: Breastfeeding Success: Shaming or Inspiring? Formula-Feeding: Guilt or Anger? | The best season of my life
Pingback: A Downloadable Visual Birth Plan | The best season of my life
Pingback: The Fourth Trimester: Take Two | The best season of my life
Pingback: The Beauty In Bedsharing | The best season of my life
This rang so true for me; we got off to a bad start in the hospital when my son immediately screamed when he tried to latch. A tongue tie was diagnosed but by the time it had been snipped, the heavy handed efforts of the hospital staff had resulted in him having a severe breast aversion. I’ve been exclusively pumping for 15 weeks, and am both proud of myself and exhausted by it. Thanks for writing this; so many people seem to judge me for using a bottle when they don’t know the full story.
LikeLike
This sounds so much like our nursing relationship! My son was 10lbs at birth and didn’t latch on at first either. I was lucky enough to have very supportive midwives and a doula who helped me get into the LC two days after he was born. She was very helpful, but recommended trying to fix the problem with stretches rather than surgery. It was a long road of hospital grade pumping, low supply-now over supply, SNS, speech therapy, and finally an upper lip and tongue tie release at 10 weeks old. I’m so sorry you weren’t able to have the SNS early on. I’m pretty sure that saved us. I could only do it 2-3 times a day because it still hurt most of the time when he’d “latch” and it was just too much with bottle feeding/pumping. He is 14 weeks today and exclusively breastfeeding except one bottle (so he remembers how!) and my nipples are just now starting to heal! It’s still not perfect, we have a session or two a day where my Raynaud’s is triggered by a bad latch, but it’s so much better. Having had the lip/tongue done should save future speech and eating problems, too! Good job mama I know how hard it is and your baby appreciates your milk no matter how they get it!
LikeLike
Thank you So much for sharing
LikeLike
I cried. I’m still crying. As I sit here nursing my 6 mo old son, my first baby, the baby I knew from the moment I heard his heartbeat I would nurse. I cherish this moment, each one, because it is a miracle he wants anything to do with nursing as he only transfers a half oz total from both breasts after 20 min or more of nursing. You see I knew about ties, I thought I knew everything. But I didn’t know 24 hrs pp I’d be standing in a hospital hallway at 230 am with a screaming baby begging a nurse to find someone to help me get him to latch (he hadn’t done so once). I didn’t know they wouldn’t send someone to help me until the next day. I didn’t know “help” would be an inexperienced wic lc who would tell me I had flat nipples and to get a nipple sheild. I didn’t know the nurse who tried to help me would suggest dripping formula on the sheild to make my son interested in sucking instead of teaching me to hand express and syringe feed. I didn’t know the hospital would tell me they didn’t have an electic pump and that 12 hours later they would hand me a manual one with the wrong sized flange and no idea how to use it or what it should feel like. I didn’t know how to hand express or that it was the better option for colustrum. I didn’t know my baby needed to urinate after circumscision or they would try to send me home but keep him, so out of fear I started spoon feeding him formula. At 3 weeks pp I was at the ent excited and nervous to get his ties clipped and start our breastfeeding journey for real. I didn’t know the ent I saw would clip his anterior tie but miss the posterior tie and the lip tie. I didn’t know this would cause my son to lose all semblance of suck strength and pattern, even with the sheild, and to lose 2 pounds in 2 weeks. I didn’t know that all of this time, these first 5 weeks post partum that I should have been pumping, silly me, I hadn’t even bought a pump yet. Everything I had read said don’t pump before 6 weeks it will cause an oversupply. Ha! Oversupply, I wish. I didn’t know the ibclc I saw 6 weeks postpartum would be an undercover formula rep. It’s good he takes a bottle she said, limit his time at your breast to only 5 min per feed, focus on pumping she said, try these supplements that make you ill she said, don’t nurse him to sleep she said, pumping makes you miserable and depressed as your son screams for you and your output never increases that’s okay just keep pumping she said, and the icing on the cake “you will likely never have a full supply, prolactin receptors are laid down in the first 4 to 6 weeks and some people really need that early stimulation, you sought help too late.” she said. So as I sit here nursing my son after having pumped 5 ml (my normal pump output missed feed or not). As I look down at his head pillowed on my breast and his sleep smile, I mourn the loss of my goal of full term breastfeeding. As I prepare his 4 oz bottle (one of 5 he gets a day) I despise myself for only registering for 3 bottles total and never researching formula. I scrunch my nose at the smell of formula on his clothing and neck and can’t wait until I take him in the shower with me to rinse it away and not have to smell it for a few brief shining moments. The things I didn’t know fill me with a regret I will never fully be rid of but the things the medical professionals, who were supposed to help and guide me, didnt know fill me with an anger so strong and fierce it almost consumed my entire family. It is all I can do to keep it at bay.
LikeLike
Pingback: The end of maternity leave: The most important work | The best season of my life
Pingback: The end of maternity leave: The most important work | The best season of my life
I had to read this in parts because I have bursted into tears like you have no idea. Thank you for sharing this, thank you for your words, I can’t wait to see how it goes with your second child. I am pregnant as well, and scared to the bone as I had struggled so badly with my first daughter too. I had to quit my exclusive pumping sessions because she had a terrible CMPA and so, I had to give her Neocate. I am not feeling as confident as you are, even with all the information that we had to get so desperately, right?
My baby is expected to come in july, so I will keep reading and trying to get ready for the moment, but as you say, a numer of things could happen… what about the luck of nursing without so many problems, it’s a possibility too, right?
Thank you again.
LikeLike
Pingback: Failed by the System: A Breastfeeding Journey Part 1 | The best season of my life
Thank you so much for sharing this. As a hospital based IBCLC, I see this scenario far too often. The evidence to practice gap is wide, and unfortunately outdated practices run rampant in my community. As a mother, my second baby was born with a posterior tongue tie, bubble palate, and lip tie. It has informed my practice immensely to know how to it feels to struggle with, what feels like, an invisible problem. The time I spent seeking solutions from healthcare providers that didn’t have answers was discouraging. I’m a maternal health RN, an IBCLC, and had excellent care and postpartum follow up, and I was the only one that recognized that something was awry with our breastfeeding dynamics and I wasn’t sure what to do. I share this to say, you are not alone. There are many women who have walked this path along side you. Thank you for sharing your story, so that other women may find refuge, and that professionals may find inspiration to provide more sensitive and thorough assessment and care. You are a wonderful mother.
LikeLike
I am having a very similar experience like yours. Thank you so much for sharing your story and it makes me strong again and confirm pumping is sustainable unlike what all those midwife or health visitor said.
I was totally let down by the NHS system. My DD have a good latch but she lose 12% weight on day 2 and jaundice made her impossible to breastfeed as she fall asleep constantly. In order to boost her weight. We used formula and expressed milk in bottle. A midwife told us she have a very minor tongue tie but not worthy to have treatment, so I keep blaming myself it must be my breastfeeding technique or position goes wrong therefore she never settle on my breast.
Around week 2, we found out she actually have quite a serious tongue tie from a doula who have no medical background. However, it was too late as she already developed nipple confusion. The doula taught us pace bottle feeding, using nipples shield and we purchased the supplementer. However, the lack of sleep, seeing screaming baby all the time put me on the edge of having postnatal depression.I gave up offering her breast for a week now but will try again with the supplementer, hopefully miracle will happen.
Hope your 2nd pregnancy have a good breastfeeding journey and both you and baby have very good health.
LikeLike